By Benjamin Boettner, Wyss Institute for Biologically Inspired Engineering at Harvard August 4, 2024
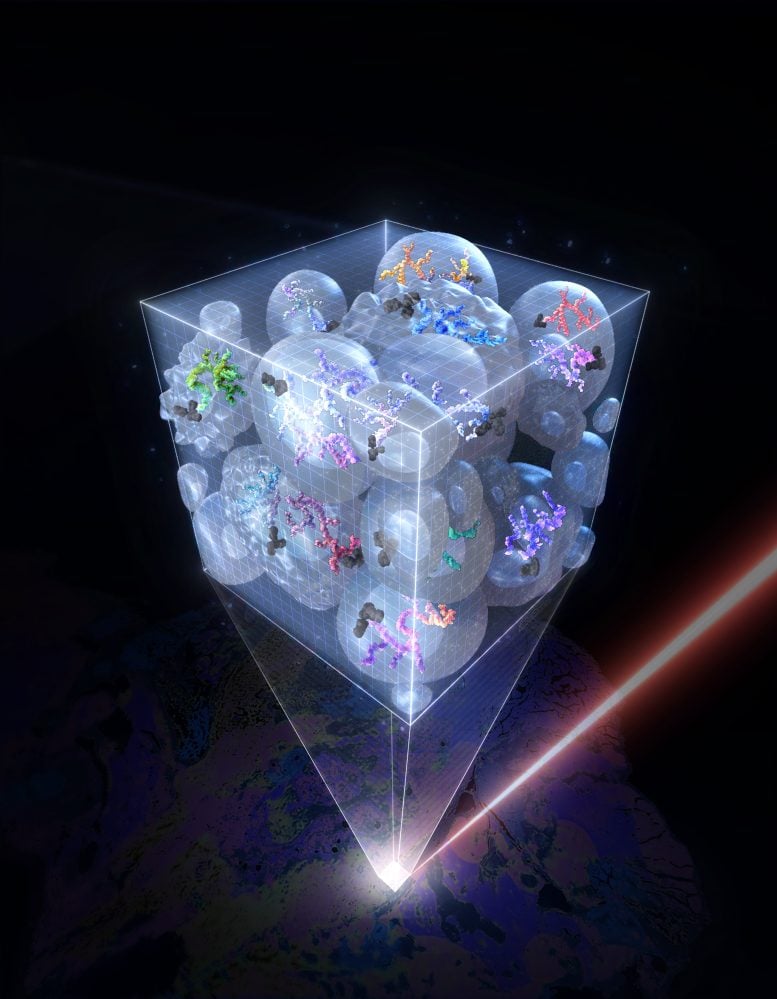
ACE technology enables highly multiplexed and sensitive signal amplification to detect proteins in single cells using suspension mass cytometry single-cell suspension and imaging mass cytometry analysis. This illustration shows how proteins in individual cells of a tissue section can be quantified with ACE-enhanced antibodies binding to them. Credit: Su Min Suh/SciStories
ACE, a groundbreaking mouse breast cancer cells multiple times during their 28-day transition from an epithelial to a mesenchymal state and back, and computationally parsing the results, they were able to shed new light on the two processes. “ACE allowed us to profile levels of low-abundance transcription factors simultaneously with markers reflecting cellular physiological and signaling states in single cells. This led to a more refined picture of how molecular programs in EMT and MET are driven by increasing and decreasing amounts of key transcription factors, including Zeb-1 and Snail/Slug,” said Sheng.
In their second example, they zoomed into the inner workings of single T cells. The stimulation of T-cell receptor (TCR) molecules on their surface results in the activation of a complex network of intracellular signaling proteins. Analyzing these signaling responses at single-cell resolution has been difficult, also due to T cells’ small size. Individual proteins of this network are activated by phosphate residues that are attached to them by other network proteins generally known as kinases. Many of these activated network proteins go on to phosphorylate other proteins of the network. This ultimately leads to changes in T-cell behavior, for example, toward pathogens or cancer cells. The researchers applied ACE to a panel of 30 antibodies that specifically bound to phosphorylated motifs in TCR-network proteins with functions in stress, inflammation, cell proliferation, and other responses. “Using ACE-enhanced mass cytometry analysis, we captured quantitative snapshots of the dynamically changing TCR network in individual primary human T cells. This allowed us to study the single-cell variations in the timing and duration of specific T-cell activation events and to reveal how the network is activated from its ground state by extracellular cues,” said Lun.
The team used the same ACE-enhanced antibody panel to investigate a phenomenon known as “injury-induced T-cell paralysis.” T cells experiencing injury in their environment, such as tissue injuries caused in major surgical procedures, often become immunosuppressive. To start to understand how the TCR network causes this, Yin’s group collaborated with co-author Michael Yaffe, M.D., Ph.D., who is the David H. Koch Professor of Science and Professor of Biology and Biological Engineering at MIT and has a strong interest in how the microenvironment surrounding sites of tissue injury suppresses the immune system. Yaffe provided the team with samples of “postoperative drainage fluid” (POF) that were obtained from patients undergoing surgery. Stimulating T cells with POFs as well as their TCRs enabled the researchers to isolate distinct network changes that cause single T cells to stop dividing and become exhausted.
Finally, they investigated the utility of ACE also for spatial analysis of proteins in tissue sections using IMC by focusing on the human kidney. Kidney tissue is difficult to analyze by fluorescence microscopy because of its strong autofluorescence, and by traditional IMC because it lacks sensitivity. The researchers developed a panel of 20 ACE-enhanced antibodies for various kidney markers and used it to examine sections of the renal cortex derived from a patient with polycystic kidney disease. This approach, in which they collaborated with co-author Hartland Jackson, Ph.D., Professor at the University of Toronto, Canada and expert in multiplexed imaging, allowed them to identify the different cell types and their organization within the kidney’s proximal and distal tubules, collecting ducts, and blood-filtering glomeruli. “We discovered new disease-specific features of cell and tissue organization and found that the stem cell marker Nestin, which is also associated with kidney disorders, was expressed very heterogeneously across glomeruli,” said Lun. “This could mean that different parts of the tissue could be simultaneously going through different pathological stages.”
“This new mass cytometry approach developed by Peng Yin’s team and their collaborators once again shows the power of leveraging DNA nanotechnology to turbocharge an existing technique that is highly relevant for clinical care, and to bring it to a much higher level of sensitivity and specificity. This relatively simple method will lead to entirely new insights into cell, tissue, and organ function, both during health and disease,” said co-senior author and Wyss Founding Director Donald Ingber, M.D., Ph.D., whose group provided critical expertise on stimulating T cells. He is also the Judah Folkman Professor of Vascular Biology at HMS and Boston Children’s Hospital, and the Hansjörg Wyss Professor of Bioinspired Engineering at the Harvard John A. Paulson School of Engineering and Applied Sciences.
Reference: “Signal amplification by cyclic extension enables high-sensitivity single-cell mass cytometry” by Xiao-Kang Lun, Kuanwei Sheng, Xueyang Yu, Ching Yeung Lam, Gokul Gowri, Matthew Serrata, Yunhao Zhai, Hanquan Su, Jingyi Luan, Youngeun Kim, Donald E. Ingber, Hartland W. Jackson, Michael B. Yaffe and Peng Yin, 29 July 2024, Nature Biotechnology.
DOI: 10.1038/s41587-024-02316-x
Other authors on the study are Xueyang Yu, Ching Yeung Lam, Gokul Gowri, Matthew Serrata, Yunhao Zhai, Hanquan Su, Jingyi Luan, and Youngeun Kim. The study was supported by grants from the